12 Interface Clinical Services Strategies To Boost Efficiency

The healthcare industry is undergoing a significant transformation, driven by the need for improved patient outcomes, enhanced patient experience, and reduced costs. At the heart of this transformation is the optimization of clinical services, which can be achieved through the implementation of effective interface clinical services strategies. These strategies focus on streamlining clinical workflows, improving communication between healthcare providers, and leveraging technology to enhance patient care. In this article, we will explore 12 interface clinical services strategies that can help boost efficiency in healthcare organizations.
Introduction to Interface Clinical Services

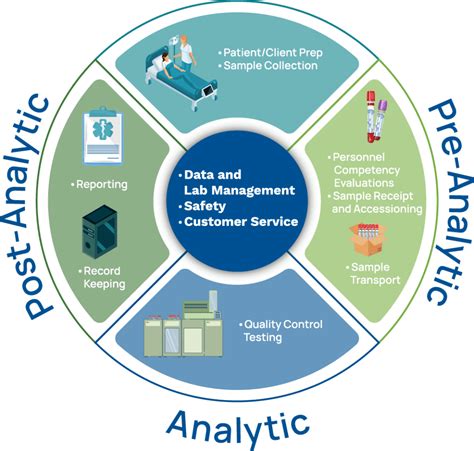
Interface clinical services refer to the interactions and exchanges between different healthcare providers, patients, and systems. These interfaces can be physical, such as face-to-face interactions between healthcare providers, or virtual, such as electronic health record (EHR) systems. Effective interface clinical services strategies are critical to ensuring seamless communication, reducing errors, and improving patient outcomes. By implementing these strategies, healthcare organizations can enhance the quality of care, reduce costs, and improve patient satisfaction.
Strategy 1: Implement Electronic Health Records (EHRs)
Electronic health records (EHRs) are a crucial component of interface clinical services. EHRs enable healthcare providers to access and share patient information electronically, reducing the need for paper-based records and improving communication between providers. EHRs can also help reduce medical errors by providing real-time access to patient information, medication lists, and allergy information. Furthermore, EHRs can facilitate the sharing of patient information between different healthcare providers, reducing the need for redundant testing and improving continuity of care.
| Benefits of EHRs | Description |
|---|---|
| Improved Communication | Enhanced communication between healthcare providers |
| Reduced Errors | Real-time access to patient information reduces medical errors |
| Increased Efficiency | Streamlined clinical workflows and reduced paperwork |

Strategy 2: Develop Clinical Decision Support Systems (CDSSs)
Clinical decision support systems (CDSSs) are computer-based systems that provide healthcare providers with clinical decision-making support. CDSSs can help healthcare providers diagnose and treat patients more effectively by providing real-time access to evidence-based guidelines, medication information, and patient data. CDSSs can also help reduce medical errors by alerting healthcare providers to potential errors and providing recommendations for alternative treatments.
Strategy 3: Implement Telehealth Services
Telehealth services enable patients to receive medical care remotely, reducing the need for in-person visits and improving access to care. Telehealth services can be particularly beneficial for patients with chronic conditions, who require regular monitoring and follow-up care. Telehealth services can also help reduce healthcare costs by reducing the need for hospitalizations and emergency department visits.
Optimizing Clinical Workflows
Optimizing clinical workflows is critical to improving efficiency in healthcare organizations. By streamlining clinical workflows, healthcare organizations can reduce waste, improve productivity, and enhance patient outcomes. The following strategies can help optimize clinical workflows:
Strategy 4: Standardize Clinical Processes
Standardizing clinical processes can help reduce variation in care and improve patient outcomes. Standardized clinical processes can also help reduce errors by providing a clear and consistent approach to patient care. Standardized clinical processes can be developed through the use of evidence-based guidelines, care pathways, and clinical protocols.
Strategy 5: Implement Lean Principles
Lean principles are a set of principles that aim to eliminate waste and improve efficiency in healthcare organizations. Lean principles can help reduce waste and improve productivity by streamlining clinical workflows, reducing unnecessary steps, and improving communication between healthcare providers. Lean principles can be applied to various aspects of healthcare, including clinical workflows, supply chain management, and patient flow.
Strategy 6: Develop Care Coordination Programs
Care coordination programs aim to improve communication and coordination between healthcare providers, patients, and families. Care coordination programs can help reduce readmissions and improve patient outcomes by providing a comprehensive approach to patient care. Care coordination programs can be developed through the use of care managers, care coordinators, and patient navigators.
| Benefits of Care Coordination | Description |
|---|---|
| Improved Communication | Enhanced communication between healthcare providers, patients, and families |
| Reduced Readmissions | Comprehensive approach to patient care reduces readmissions |
| Improved Patient Outcomes | Care coordination programs improve patient outcomes and reduce healthcare costs |
Enhancing Patient Engagement

Patient engagement is critical to improving patient outcomes and enhancing patient experience. The following strategies can help enhance patient engagement:
Strategy 7: Implement Patient Portals
Patient portals are secure online platforms that enable patients to access their medical records, communicate with healthcare providers, and manage their care. Patient portals can help improve patient engagement and empowerment by providing patients with real-time access to their medical information and enabling them to take a more active role in their care.
Strategy 8: Develop Patient Education Programs
Patient education programs aim to educate patients about their conditions, treatments, and self-care strategies. Patient education programs can help improve patient outcomes and reduce healthcare costs by providing patients with the knowledge and skills they need to manage their care effectively. Patient education programs can be developed through the use of health literacy, patient-centered care, and shared decision-making.
Strategy 9: Implement Shared Decision-Making
Shared decision-making is a process that enables patients and healthcare providers to make decisions together about patient care. Shared decision-making can help improve patient outcomes and reduce healthcare costs by providing patients with a more active role in their care and enabling healthcare providers to make more informed decisions.
Measuring and Evaluating Performance

Measuring and evaluating performance is critical to improving efficiency in healthcare organizations. The following strategies can help measure and evaluate performance:
Strategy 10: Develop Key Performance Indicators (KPIs)
Key performance indicators (KPIs) are metrics that measure performance and outcomes in healthcare organizations. KPIs can help identify areas for improvement and track progress over time by providing a clear and consistent approach to measuring performance. KPIs can be developed through the use of data analytics, quality metrics, and outcome measures.
Strategy 11: Implement Quality Improvement Initiatives
Quality improvement initiatives aim to improve patient outcomes and reduce healthcare costs by identifying and addressing areas for improvement. Quality improvement initiatives can help reduce medical errors and improve patient safety by providing a comprehensive approach to quality improvement. Quality improvement initiatives can be developed through the use of root cause analysis, failure mode and effects analysis, and plan-do-study-act (PDSA) cycles.
Strategy 12: Develop Patient Satisfaction Surveys
Patient satisfaction surveys are tools that measure patient satisfaction and experience in healthcare organizations. Patient satisfaction surveys can help identify areas for improvement and track progress over time by providing a clear and consistent approach to measuring patient satisfaction. Patient satisfaction surveys can be developed through the use of patient-reported outcomes, patient experience metrics, and satisfaction surveys.
What are the benefits of implementing interface clinical services strategies?
+The benefits of implementing interface clinical services strategies include improved patient outcomes, enhanced patient experience, reduced healthcare costs, and improved efficiency. Interface clinical services strategies can help streamline clinical workflows, improve communication between healthcare providers, and leverage technology to enhance patient care.