Decubitus Ulcer Guide: Healing Stages
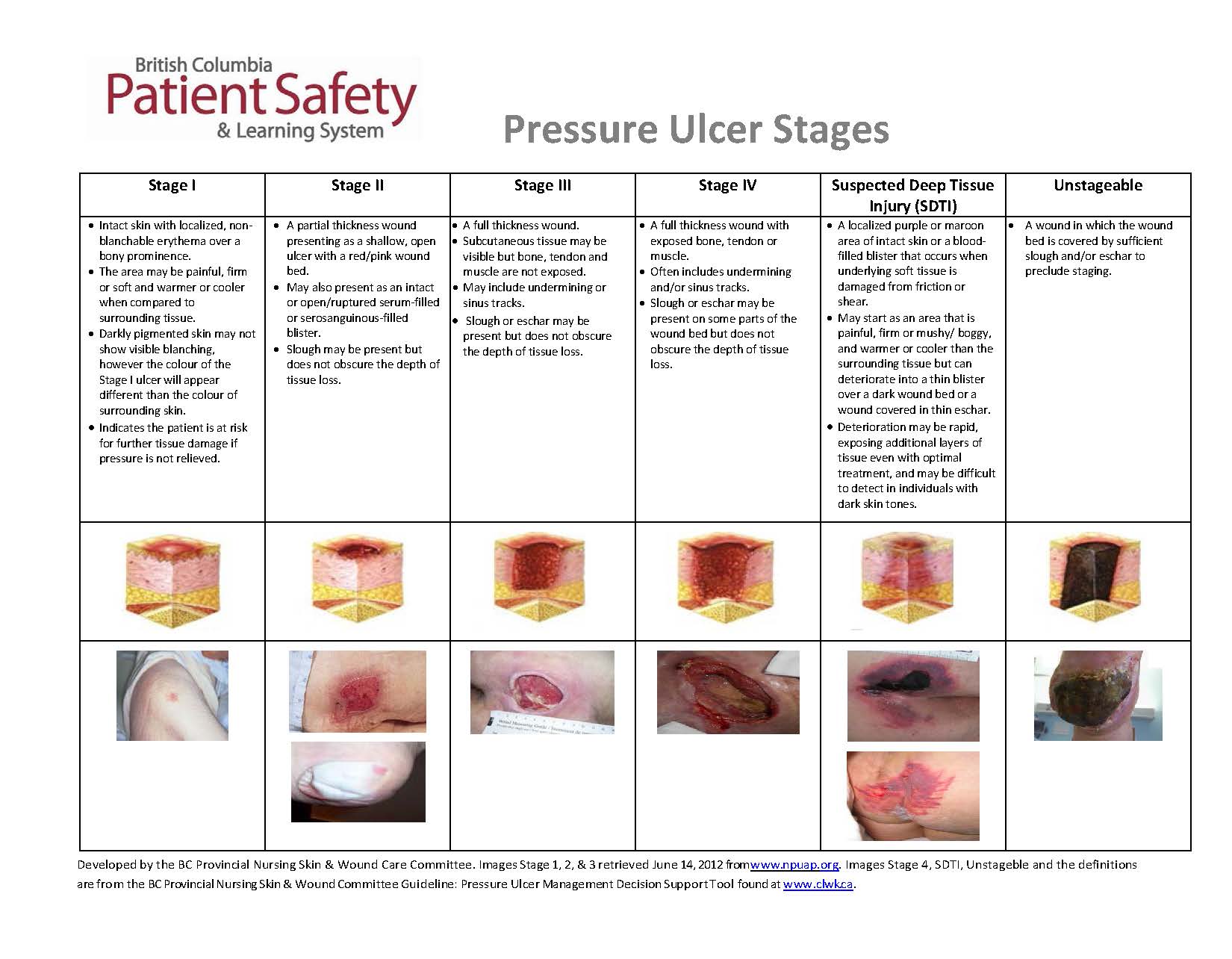
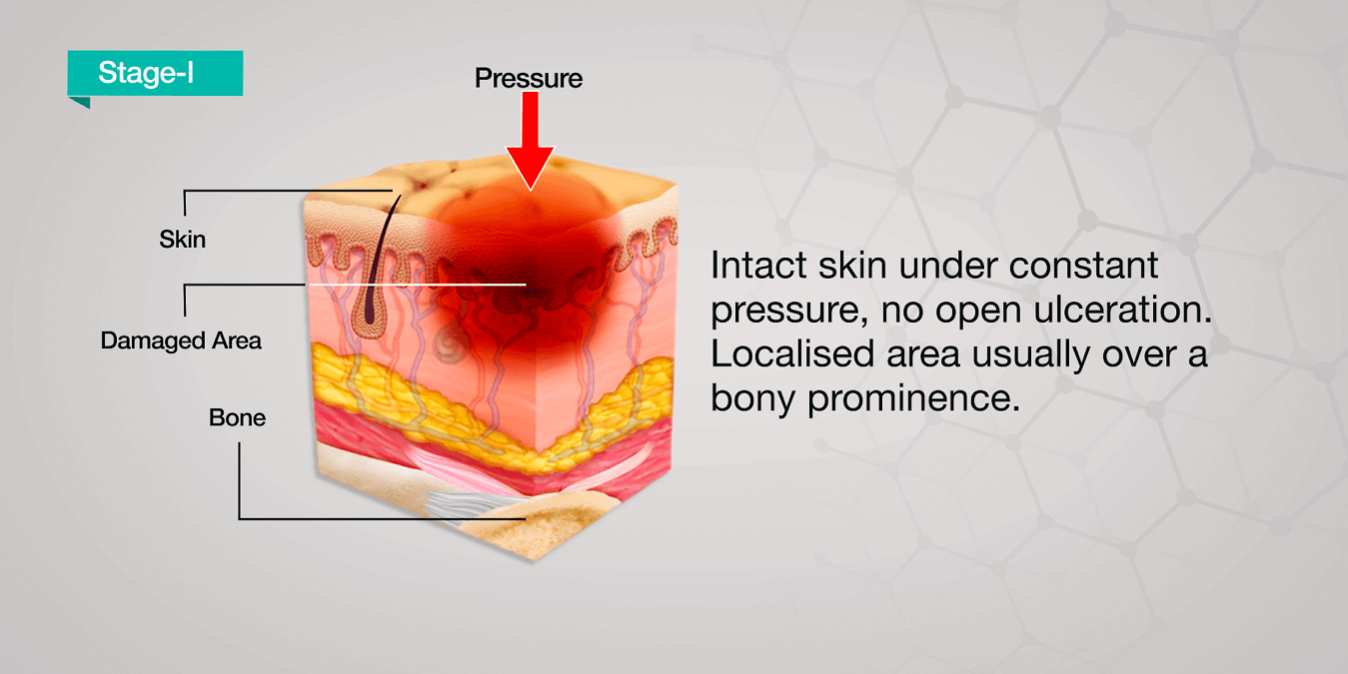
Decubitus ulcers, also known as pressure ulcers or bedsores, are localized damage to the skin and/or underlying tissue that usually occur over a bony prominence as a result of pressure, or pressure in combination with shear and/or friction. The healing process of decubitus ulcers involves several stages, each with distinct characteristics and requirements for optimal recovery. Understanding these stages is crucial for healthcare professionals and caregivers to provide appropriate care and interventions.
Introduction to Decubitus Ulcer Healing
The healing of decubitus ulcers is a complex and multifaceted process that can be influenced by various factors, including the size and depth of the ulcer, the overall health of the patient, and the effectiveness of the treatment plan. The stages of healing are generally categorized into four phases: the inflammatory phase, the debridement phase, the granulation phase, and the epithelialization phase. Each phase has specific goals and requirements for promoting healing and preventing complications.
The Inflammatory Phase
The inflammatory phase is the initial stage of the healing process, typically lasting 2-5 days. During this phase, the body’s natural response to injury is triggered, leading to increased blood flow to the affected area, swelling, redness, and warmth. The primary goal of this phase is to protect the wound from further injury and infection. Proper wound care, including cleaning and dressing the wound, is essential to promote a healthy environment for healing. The use of non-adherent dressings can help minimize trauma to the wound and surrounding tissue.
| Healing Stage | Characteristics | Duration |
|---|---|---|
| Inflammatory Phase | Increased blood flow, swelling, redness, warmth | 2-5 days |
| Debridement Phase | Removal of dead tissue, promotion of granulation tissue | Variable, depending on wound size and depth |
| Granulation Phase | Formation of granulation tissue, contraction of wound | Variable, depending on wound size and depth |
| Epithelialization Phase | Closure of wound, regeneration of epithelial tissue | Variable, depending on wound size and depth |

Debridement and Granulation Phases
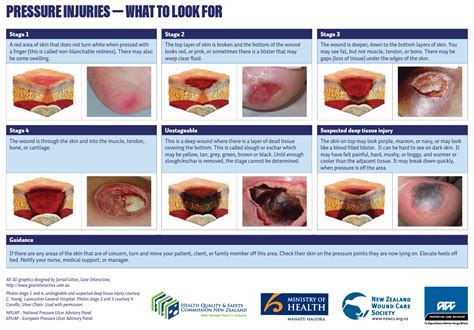
The debridement phase involves the removal of dead tissue, which is crucial for promoting the growth of healthy tissue. This phase can be facilitated through various methods, including surgical debridement, enzymatic debridement, and autolytic debridement. Following debridement, the granulation phase begins, characterized by the formation of granulation tissue, which is rich in blood vessels, collagen, and fibroblasts. This phase is critical for wound contraction and the eventual closure of the wound. Nutritional support, including adequate protein, vitamin C, and zinc, is vital for supporting the healing process during these phases.
Epithelialization Phase
The final stage of healing is the epithelialization phase, where the wound is closed through the regeneration of epithelial tissue. This phase can be influenced by various factors, including the size and depth of the wound, as well as the presence of any underlying health conditions. Wound dressings that promote a moist environment can enhance epithelialization by facilitating the migration of epithelial cells across the wound surface.
What are the key factors that influence the healing of decubitus ulcers?
+The healing of decubitus ulcers can be influenced by various factors, including the size and depth of the ulcer, the overall health of the patient, nutritional status, and the effectiveness of the treatment plan. Other factors such as mobility, hygiene, and the presence of underlying health conditions can also impact the healing process.
How can caregivers support the healing process of decubitus ulcers?
+Caregivers can support the healing process by ensuring the wound is kept clean and dressed appropriately, promoting a healthy diet rich in nutrients essential for wound healing, and encouraging regular movement and exercise to enhance blood flow and prevent further pressure injuries.
In conclusion, the healing stages of decubitus ulcers are complex and require careful management to promote optimal recovery. By understanding the characteristics and requirements of each phase, healthcare professionals and caregivers can provide targeted interventions to support the healing process and improve patient outcomes. Regular wound assessments, proper wound care, and nutritional support are critical components of a comprehensive treatment plan for decubitus ulcers.